Note: I wrote this article a few weeks ago, intending to post it later. But this morning — on the 4th of July, a day meant to celebrate independence and the so-called American spirit — it feels like there's nothing to celebrate. Trump’s “Big Beautiful Bill” has passed, and with it comes a slew of issues: millions of people left uninsured, Medicaid funding slashed, and more. As you read this, remember who gets left behind when power prioritizes profit over people. Don’t look away. Don’t forget.
The thing about me is that I’ve always been weak to marketing.
My friends can confirm this. I’ve nearly caved to buying those weird cans of green powders. During one point in the pandemic, I tried multiple different recipes for the “perfect green smoothie.” I tried magnesium for sleep but it really only functioned as a mild laxative for me. I’ve saved wellness routines from random influencers who have completely different lives and bodies than mine.
Technically, I should know better. I’m in medical school, I know about the placebo effect, the profit motives, the lack of regulation in the supplement industry, all this and more. But it’s a tempting narrative, isn’t it? The idea that with the right effort, the right product, the right habits, you could optimize your way out of suffering.
That belief isn’t accidental. It’s everywhere. And lately, it’s become something even bigger than a Pinterest board or a Tiktok-based shopping cart. It’s transformed into a political platform in line with the far right.
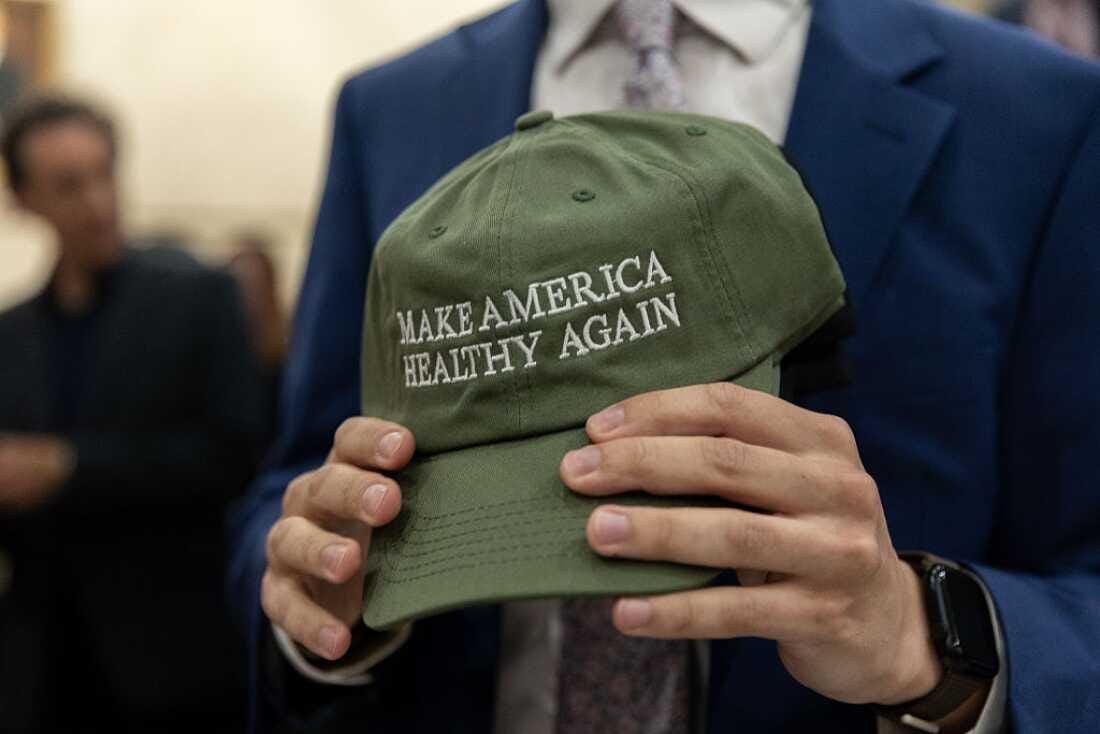
Yes, I’m talking about MAHA: “Make America Healthy Again.”
Depending on who’s using it, MAHA can mean a few things. For wellness influencers, it’s usually an aesthetic: raw milk, cold plunges, and rage-posting about seed oils. For RFK Jr., it’s a rallying cry against vaccines, public health institutions, and anything that smells like Big Pharma. And during the Trump administration, it showed up in policies that punished poor people for not being “healthy enough” to deserve care.
But the message, regardless of who’s saying it, is the same: health is a moral obligation. If you’re sick, you must have done something wrong. If you’re not optimizing, you’re failing. And if you want help, you’d better prove that you deserve it. This isn’t just about MAHA as a phrase. Rather, it’s about what happens when we treat health like a test of character, and more importantly, what gets left behind when we do.
What is MAHA?
In case you didn’t know, MAHA stands for “Make America Healthy Again,” riffing off of Trump’s presidential campaign slogan of “Make America Great Again.” It’s certainly a catchy saying, and at first glance, it might seem relatively harmless. However, this slogan — and the rest of the MAHA movement as a whole — is about control.
It was popularized by Robert F. Kennedy Jr., now serving as Trump’s Secretary of Health and Human Services. After suspending his botched independent presidential campaign in 2024, he aligned himself with Trump. His version of MAGA pushes “natural” health, distrusts public health infrastructure, and blames chronic illness on toxins, seed oils, and childhood vaccines.
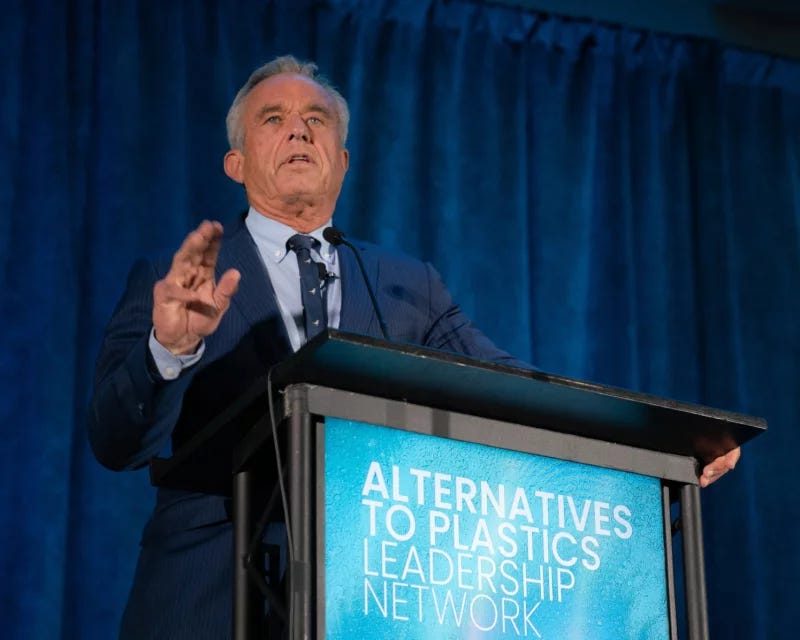
Kennedy’s version of MAHA is part libertarian health fantasy, part Instagram wellness spiral. It’s obsessed with “toxins,” food additives, and childhood vaccines. It elevates “natural living” to a kind of sacred obligation while vilifying anything remotely institutional — the CDC, the FDA, pediatricians. In this world, chronic illness isn’t a complex interplay of genetics, social determinants, and environmental exposures — it’s a personal failing. And you, the flawed individual, can supposedly fix it all through filtered water and gut health protocols.
Yet, while MAHA preaches clean eating and detox protocols, the Trump administration has proposed slashing Medicaid and cutting public health funding, all under the banner of “freedom.” 1,2 RFK Jr. loves to talk about chronic illness and how we need to focus on that, but since he started as Secretary of Health, significant programs and grants focusing on research on diabetes, dementia, kidney disease, and more have all been cut 3. The NIH has also cut studies about ways to improve trust in vaccines and accessibility to vaccination, all while measles outbreaks continue amongst unvaccinated children 4,5.
If you can’t afford care? Start juicing. If you’re disabled or chronically ill? Try harder. This is what happens when you turn health into a moral litmus test: the sick become disposable, and the system absolves itself of responsibility. You’ll hear a lot of buzzwords: sovereignty, detoxing, resilience. But at its core, MAHA tells a story as old as American individualism, one where health is a personal virtue and illness is a personal failure. And if you can’t bootstrap your way out of it? You’ve clearly done something wrong.

From public health to public panic
To be clear, the idea that you should “take responsibility” for your health is not new. For decades, public health in America has prioritized individual behavior change — diet, exercise, smoking cessation — as a substitute for addressing structural conditions like poverty, housing, and unequal access to care 6–8. It’s easier to tell people to walk more than to build safe neighborhoods to walk in. It’s the wellness version of bootstrapping.
This shift has been heavily politicized by the current administration. MAHA tells people to take their supplements and skip their yearly vaccines while the administration slashes Medicaid and guts public health infrastructure. It’s a bait-and-switch: public investment in health is framed as government overreach, while wellness becomes something you have to privately achieve (and buy).
This isn’t a new playbook, but MAHA has made it louder and meaner. It recasts collective failures as individual ones. It positions institutional distrust as enlightenment. Getting vaccinated is blind obedience while drinking raw milk is liberation. Trusting doctors makes you a sheep while biohacking your way to inner purity makes you free.
This is what MAHA offers: health as a moral imperative and a system that quietly abandons the bodies that don’t fit.
That’s precisely where the cruelty of this movement comes in. It’s the complete erasure of context that is so devastating to me. Disability, poverty, trauma, structural racism — none of that matters. Health becomes a meritocracy where you get what you deserve. Meanwhile, the actual building blocks of public health — clean water, prenatal care, safe housing, reliable access to medication — gets pushed to the margins in favor of trend cycles and fear. The conversation has shifted from “how do we keep people well?” to “how do we make sure only the right people get care?”
Granted, medical bias and discrimination has existed well before RFK Jr.’s appointment. In clinical settings, patients are routinely judged — consciously or not — on how much they “deserve” care. Fat patients are told to lose weight before being taken seriously 9. Poor patients are labeled “noncompliant.” 10,11 Black patients receive less pain medication and are less likely to be referred for specialty care 12. The implication, where some people are worth saving while others are worth blaming, has always been there. But now, it’s not just an undercurrent. It’s being formalized as political strategy.
When those same biases are codified into national health policy, the damage compounds. It shifts medicine away from equity and towards enforcement. Funding gets cut, safety nets shrink, and research stalls. Care becomes a reward for the “disciplined” and a punishment for the “noncompliant.” And because this ideology cloaks itself in wellness rhetoric — personal responsibility, clean living, “natural” health — it’s harder to challenge. It sounds empowering until it’s used to deny you coverage.
The long-term consequences of politicizing health this way are — and have been — devastating. Public health becomes fragmented and privatized 13,14. Chronic illness outcomes worsen. Vulnerable patients delay care or avoid the system altogether, leading to more late-stage diagnoses and preventable deaths 15. Trust in medical institutions erodes, not because of some anti-science conspiracy, but because the system actually fails the people who need it most 16–18.
The Trump administration’s involvement doesn’t just legitimize this ideology. It weaponizes it. It transforms lifestyle preference into federal policy. It transforms social stigma into bureaucratic criteria. And it reinforces the idea that health isn’t a shared good — it’s something you earn, and if you can’t? You’re on your own. That’s the real harm. Not just misinformation, but infrastructure.
What we deserve
And I get it. Like I said, I still fall for it sometimes: the green powders, the gut health hacks, the idea that if I just tried harder, I could feel better. But the personal pursuit of health doesn’t exist in a vacuum. It exists in a country where care is conditional, where systems are being dismantled in real time, and where wellness is being wielded as a weapon.
MAHA isn’t about making people healthy. It’s about making health harder to access unless you look, act, and live a certain way. It’s not self-improvement; it’s sanctioned exclusion, wrapped in leafy greens. We don’t need more detox plans or influencers. We deserve public infrastructure and policy that will actually care for people, not just those that fit the mold.
MAHA will not save us — because health isn’t a virtue. It’s a human right. And no amount of raw milk or green powder is going to fix a system designed to fail the most vulnerable.

Additional articles to read
“Asbestos, Measles, Coal Plants: How Kennedy and Trump Are Making America “Healthy” Again” by Bess Levin
“The Wellness Women Are on the March” by Elaine Godfrey
“The Cancer Scams that Foreshadowed MAHA” by Jessica Winter
“The Pilates Princess to Diet Culture Pipeline” by Jordan Theresa (video essay)
“almond moms and the cult of generational diet culture” by Rowan Ellis (video essay)
“RFK Jr’s ‘Maha’ report found to contain citations to nonexistent studies” by Joseph Gedeon
References
Sanger-Katz M, Kliff S. Republicans Pass Strictest Medicaid Work Requirement They’ve Ever Put Forward. New York Times. https://www.nytimes.com/2025/05/22/upshot/medicaid-republicans-work-requirement.html. May 22, 2025.
Lapowsky I. Trump’s Real MAHA Agenda: More Leafy Greens, Less Health Care. Vanity Fair. https://www.vanityfair.com/news/story/trump-rfk-maha-report-spending-bill?srsltid=AfmBOopC12Zm1TLjifP7V5yVNKlQ4KpzZCdOZj7dXo-xzOvY_36VQ3wa. May 23, 2025.
Kolata G. As Kennedy Champions Chronic Disease Prevention, Key Research Is Cut. New York Times. https://www.nytimes.com/2025/04/07/health/rfk-hhs-diabetes-obesity-disease.html. April 7, 2025.
Neergaard L. Researchers are learning the Trump administration axed their work to improve vaccination. AP News. https://apnews.com/article/vaccine-trump-research-cuts-nih-e6d7d79bdf08375b826b06d14f856cf7. March 11, 2025.
The Associated Press. RFK Jr. made promises about vaccines. Here’s what he’s done as health secretary. AP News. https://apnews.com/article/rfk-vaccine-policies-promises-d1ad570053583d953f15ec3e566e426f. June 27, 2025.
Adler NE, Cutler DM, Fielding JE, et al. Addressing Social Determinants of Health and Health Disparities: A Vital Direction for Health and Health Care. NAM Perspect. 2016;6(9). doi:10.31478/201609t
Pampel FC, Krueger PM, Denney JT. Socioeconomic Disparities in Health Behaviors. Annu Rev Sociol. 2010;36(1):349-370. doi:10.1146/annurev.soc.012809.102529
Woolf SH, Braveman P. Where Health Disparities Begin: The Role Of Social And Economic Determinants—And Why Current Policies May Make Matters Worse. Health Aff (Millwood). 2011;30(10):1852-1859. doi:10.1377/hlthaff.2011.0685
Phelan SM, Burgess DJ, Yeazel MW, Hellerstedt WL, Griffin JM, Van Ryn M. Impact of weight bias and stigma on quality of care and outcomes for patients with obesity. Obes Rev. 2015;16(4):319-326. doi:10.1111/obr.12266
Gordon HS, Street RL, Sharf BF, Souchek J. Racial differences in doctors’ information‐giving and patients’ participation. Cancer. 2006;107(6):1313-1320. doi:10.1002/cncr.22122
Kaplan SH, Greenfield S, Ware JE. Assessing the effects of physician-patient interactions on the outcomes of chronic disease. Med Care. 1989;27(3 Suppl):S110-127. doi:10.1097/00005650-198903001-00010
Vargas A, Tobey-Moore L, Curran G, et al. Exploring Racial Disparities in Chronic Pain Management. J Pain Res. 2025;Volume 18:2901-2908. doi:10.2147/JPR.S493664
Thomson DR, Amoroso C, Atwood S, et al. Impact of a health system strengthening intervention on maternal and child health outputs and outcomes in rural Rwanda 2005–2010. BMJ Glob Health. 2018;3(2):e000674. doi:10.1136/bmjgh-2017-000674
Brown TM, Cueto M, Fee E. The World Health Organization and the transition from “international” to “global” public health. Am J Public Health. 2006;96(1):62-72. doi:10.2105/AJPH.2004.050831
Freeman HP. Poverty, Culture, and Social Injustice: Determinants of Cancer Disparities. CA Cancer J Clin. 2004;54(2):72-77. doi:10.3322/canjclin.54.2.72
Baum F, Fisher M. Why behavioural health promotion endures despite its failure to reduce health inequities. Sociol Health Illn. 2014;36(2):213-225. doi:10.1111/1467-9566.12112
Kavanagh MM, Singh R. Democracy, Capacity, and Coercion in Pandemic Response: COVID-19 in Comparative Political Perspective. J Health Polit Policy Law. 2020;45(6):997-1012. doi:10.1215/03616878-8641530
Blendon RJ, Benson JM, Hero JO. Public Trust in Physicians — U.S. Medicine in International Perspective. N Engl J Med. 2014;371(17):1570-1572. doi:10.1056/NEJMp1407373